£79.00
Do you think you might be approaching the menopause?
Are you suffering from symptoms such as hot flushes, anxiety, night sweats, poor sleep and low energy?
Find out more about your menopause status.
- Tests for LH, FSH and oestradiol which are key markers of menopause status
- Simple at-home finger-prick blood test. No social interaction required
- Provides hospital standard, easy-to-read results
- Provides clear information as to whether or not your results indicate peri-menopause or menopause
- Includes lifestyle advice to better support your health
- Ideally suited for women who are approaching menopausal age
- Not suitable for those taking hormonal contraception or hormone replacement therapy
- Only available in the UK
† please note, the price shown includes a currency conversion fee of 5% on non-GBP transactions.
Optimise Your Health At Home.
Take control of your health in a positive way. Understand whether your menopause status may be impacting your health and what you can do to help yourself.
Using a quick and easy home-to-laboratory finger-prick blood test. Get your results within 7 days.
Being aware of your menopause status is the first step to making positive changes. It is also easy to track your hormone levels over time.
Take steps to change your life for the better.
Measuring your menopause status is important, particularly if you……
- want to know more about what might be impacting your health and be ready to take on whatever comes your way
- experience hot flushes
- suffer from night sweats
- wonder if you are going through early menopause
- have trouble sleeping
- suffer from mood changes / anxiety
- have erratic periods
- are intrigued to find out more
How It Works
1.
Place your order, and we’ll post it to you directly.
2.
Take a finger prick test and collect 2-3 drops of blood, and post back to our laboratory.
3.
Receive and review your results, in a simple, easy to understand way.
What We Test For
LH and FSH
LH and FSH are hormones produced by the pituitary gland in the brain. These hormones are responsible for ensuring the normal function of the ovaries and the menstrual cycle.
Oestradiol
Oestradiol is the main form of oestrogen, and it is produced by the ovaries.
FAQ’s
What is the menopause?
Menopause occurs when the ovaries have few remaining eggs and can no longer produce oestrogen and progesterone. Typically, periods become less frequent over a few months or years and then stop completely. For some women, periods come to a sudden rather than gradual stop.
For most women, the menopause is a natural part of getting older. Some women reach menopause before they’re 45, which is called early menopause. Before the age of 40, it’s known as premature menopause. Late menopause is possible but 80% of women will have stopped having periods by the age of 54.
Some treatments, surgeries and conditions can bring about the menopause, such as:
chemotherapy or radiotherapy
oophorectomy – removal of the ovaries (often at the time of a hysterectomy)
underlying conditions for example genetic abnormalities and Addison’s disease
anti-oestrogen hormone therapy
Reaching menopause technically means you’ve had no consecutive periods for 12 months. But menopausal symptoms include anything that you may experience before your periods start to change, during the time your hormone balance starts to affect the pattern of your periods (perimenopause), and the postmenopausal stage – when your periods have stopped for more than a year.
What are the symptoms?
The first sign of menopause is usually a change in the pattern of your periods. They may be lighter or heavier than they are normally, and the frequency is likely to change. You may have a period every few weeks or months.
Period pattern changes are not the only sign that you’re approaching menopause. The majority of women will have some menopause symptoms at some stage, even before experiencing changes in their periods.
It’s common to experience a range of menopause symptoms, including:
Hot Flushes (Also Called Hot Flashes)
What Do Hot Flushes Feel Like?
Hot flushes (also known as hot flashes) are a sudden feeling of intense heat that spreads through the body. They can cause redness in your face, neck and chest, as well as sweating and palpitations (when your heart feels like it’s pounding, fluttering or beating more irregularly than usual).
Hot flushes typically last for a few minutes. You might have them only mildly or occasionally, and not be troubled by them. But for some menopausal women they can be frequent, sometimes happening several times a day. They can be uncomfortable and embarrassing.
Hot flushes may start months or years before you reach menopause, and many women find they continue for months or years after their periods stop.
What’s The Cause Of Hot Flushes?
Hot flushes are a type of reaction called vasomotor – which means that changes in your hormone levels affect the way your body controls its temperature.
Is There Any Treatment For Hot Flushes?
Hormone replacement therapy (HRT), which replaces the oestrogen your body stops producing at menopause, can relieve many menopause symptoms including hot flushes. You can take oestrogen in the form of tablets, skin patches, gels or implants.
Other than HRT, the treatment for hot flushes is a matter of easing the symptoms and, if possible, identifying if there are any triggers for you. It’s also worth talking to your doctor about any medicines you’re taking, if you’re concerned they may be bringing on hot flushes or making them worse.
Some things that you can try:
– Keeping coffee and tea to a minimum
– Cutting down on alcohol
– Eating mild rather than spicy foods
– Wearing loose, thin layers and opting for cottons and linens rather than synthetic fabrics
– Having cool or lukewarm showers and baths
– Sipping cold drinks throughout the day – and carrying a bottle of water with you when you go out
– Spraying or misting some water on your face when you feel a hot flush coming on
For some women, complementary therapies may help manage hot flushes, such as isoflavones or black cohosh. It’s important to talk to your doctor before you try these, as they can have side effects and interfere with some medicines.
Night Sweats – Hot Flushes At Night
What Do Night Sweats Feel Like?
Night sweats are intense feelings of heat and sweatiness that happen during the night. Just like hot flashes, they’re a sudden spreading of heat through the body. You may wake up feeling very hot with your bedding and pyjamas drenched in sweat.
It can be difficult to sleep through the night and to get enough rest when you experience profuse sweating at night. This can lead to tiredness and irritability during the day, as well as trouble focusing.
What Causes Night Sweats In Menopause?
The cause of night sweats is the same as hot flushes – a problem with how your body regulates its temperature. They can happen even if your bedroom is cool and you’re wearing light nightwear.
Though they’re generally unpredictable, night sweats may be brought on by many of the same triggers as hot flashes during the day, such as spicy foods, caffeine and smoking.
Is There Any Treatment For Night Sweats?
HRT may relieve nighttime sweating and other menopause symptoms by restoring the oestrogen your body is not producing anymore.
While they can still happen even if your bedroom is cool, there are some things you can do to feel better when night sweats happen:
Have an electric fan ready to switch on if you need it during the night
Use layers of sheets as bedding rather than a duvet, so that you can remove sheets as you need to
Keep a glass of water and a water spray by your bed
It may also be helpful to avoid the same things that can bring on hot flushes during the day. See the full list of potential triggers above and talk to your doctor if you’re worried about any medications you’re taking.
Vaginal Atrophy
What Does Vaginal Atrophy Feel Like?
Vaginal atrophy (or atrophic vaginitis) is when your vaginal walls become thinner, dryer, and inflamed, and it’s very commonfor many women duto experience this during perimenopause and after menopause.
It can lead to a range of signs and symptoms such as:
Vaginal dryness – a drop in your usual moisture level
Burning sensation in the vagina or around the vulva
Itching and redness of the vulva
Pain or discomfort during sexual intercourse
Spotting (light vaginal bleeding) after sexual intercourse
Pain or burning with urination
More frequent urinary tract infections
Urinary incontinence
Because the wide range of symptoms doesn’t just affect the vagina, but also the vulva and urinary tract, it’s sometimes known as vulvo-vaginal atrophy (VVA) or Genitourinary Syndrome of Menopause (GSM).
What Causes Vaginal Atrophy?
Vaginal atrophy can happen when your body starts producing less oestrogen at menopause. Without the hormone nourishing the tissue of your vagina, it thins and dries out, becoming less elastic and more easily hurt and inflamed.
Not all women experience this at menopause but many do, and it can carry on for years after your periods stop. It’s estimated that almost half of postmenopausal women experience some symptoms caused by vaginal atrophy.
Can You Treat Vaginal Atrophy?
Replacing the oestrogen in your body through HRT, in the form of tablets or patches, can relieve vaginal atrophy and other menopausal symptoms. If taking oestrogen in this way (affecting your whole body) does not suit you, you can apply it topically, using an oestrogen ring, cream or pessary inserted into the vagina.
There are some other things you can do to reduce the common symptoms and feel more comfortable, such as:
Using moisturisers or water-based lubricants to help relieve dryness. Vitamin E oil can also be used as a vaginal lubricant
Wearing cotton underwear and loose-fitting clothing, which can help air circulate around the genitals, making them a less ideal environment for bacteria to grow
Taking vitamin D, which can increase moisture in the vagina. It also helps the body absorb calcium, which can help guard against menopause-related weak bones
Regular sexual activity. Though it does not affect your hormone levels, sexual activity (either with or without a partner) can increase blood flow to your genitals, which can help keep vaginal tissues healthy
If you’re struggling with persistent vaginal atrophy symptoms that are affecting your daily life, see your doctor. It can be hard to talk about but there are things that can help, and you don’t have to struggle through uncomfortable symptoms on your own.
It’s common to experience a range of other menopause symptoms, including:
– Difficulty sleeping
– Tiredness and irritability
– Problems with memory, concentration and decision making – some women describe this feeling as ‘brain fog’
– Low mood or anxiety
– Reduced sex drive (libido)
– Sore breasts
– Weight gain
– Redistribution of weight/change of body shape
For most women, the menopause is a natural part of getting older. Some women reach menopause before they’re 45, which is called early menopause. Before the age of 40, it’s known as premature menopause. Late menopause is possible but 80% of women will have stopped having periods by the age of 54.
Some treatments, surgeries and conditions can bring about the menopause, such as:
chemotherapy or radiotherapy
oophorectomy – removal of the ovaries (often at the time of a hysterectomy)
underlying conditions for example genetic abnormalities and Addison’s disease
anti-oestrogen hormone therapy
Reaching menopause technically means you’ve had no consecutive periods for 12 months. But menopausal symptoms include anything that you may experience before your periods start to change, during the time your hormone balance starts to affect the pattern of your periods (perimenopause), and the postmenopausal stage – when your periods have stopped for more than a year.
What is perimenopause?
Perimenopause is the stage of hormone imbalance that can start while you are still having normal periods. It is more typically defined as the stage between having regular periods and your periods stopping altogether. It can last for a few months or for years.
During perimenopause, the levels of hormones in your body such as oestrogen, progesterone, and follicle-stimulating hormone (FSH) will change and they may fluctuate for a time. The overall fall of oestrogen means your menstrual cycle may get shorter or longer for a time before stopping.
It’s important to remember that as long as you’re still having periods, and indeed after your periods have stopped for up to a year, you can still get pregnant. If you want to prevent pregnancy you need to use contraception until you’ve had no periods for 12 months and have officially reached menopause.
How do you cope with symptoms?
Some menopausal symptoms can be severe and difficult to cope with. Society is gradually becoming more open about how menopause affects women, but many still find it hard to talk about and could be embarrassed asking for help.
It’s important to talk to your GP if you’re struggling, or finding that how you feel is interfering with your life, work and relationships. There are things that can help you manage the symptoms and find your way through the menopause more comfortably, such as:
Hormone Replacement Therapy (HRT)
Hormone replacement therapy (HRT) can relieve symptoms by replacing the oestrogen that your body is no longer producing. You can take oestrogen in the form of tablets, skin patches, gels or implants.
Starting HRT when you experience signs and symptoms can be a great help for some women. GPs will usually advise women experiencing early or premature menopause to take HRT until they reach the average age of menopause. This can help manage perimenopause symptoms and protect your bones from the risk of osteoporosis.
It’s important to bear in mind that long-term use of HRT carries some risks of side effects. However, these risks are small and will depend on how long you undergo HRT for, as well as your own health status. Your GP will advise you on whether HRT is right for you and will outline the risks in detail for you.
Healthy Diet
Many women experience menopause weight gain due to the drop in oestrogen levels and age-related loss of muscle tissue. Following a balanced diet (that includes plenty of fruits, vegetables, whole grains and complex carbohydrates without too much added sugar and saturated fat) can help you control your weight and feel better. Keeping control of your sugar levels is vital and sugary and processed foods should be avoided. Some women find that certain foods trigger hot flushes, such as hot drinks, spicy foods and alcohol, so it can be worth limiting these.
Regular Exercise
Keeping fit, active and strong can lift your mood, boost your energy levels and help you sleep. Regular exercise can also guard against osteoporosis, Diabetes and other conditions. Joining a group gym class or a running club can help if you’re struggling to feel motivated.
Don’t Smoke
Smoking can trigger hot flushes, and it also increases your risk of health problems such as heart disease, stroke, osteoporosis and cancer. For help to quit smoking, visit the NHS Website.
Medications For Osteoporosis
Doctors may recommend medication to prevent or treat osteoporosis if that’s appropriate for you. There are medications available that help reduce bone loss and the risk of fractures. Your doctor might also prescribe vitamin D supplements to help strengthen bones.
Keeping Cool
You might find it beneficial to dress in thin layers and opt for cotton and linens rather than synthetic fabrics. It’s a good idea to carry a bottle of water with you, along with anything else that helps you feel more comfortable such as a water spray, a pocket fan or wet wipes.
Vaginal Creams, Pessaries And Lubricants
These can relieve the vaginal dryness that many women experience as a result of a drop in oestrogen. They deliver a small amount of the hormone directly to the vagina, and can help if you’re experiencing painful sex or urinary discomfort.
Relaxation Techniques
Techniques such as massage, mindfulness, meditation and deep breathing may be helpful for some women. Taking some deep breaths when you feel a hot flush coming on can help it pass more quickly.
Low-Dose Antidepressants
Some studies have suggested that low doses of SSRIs (selective serotonin reuptake inhibitors), a type of antidepressant, can help reduce hot flushes and night sweats. This might be an appropriate option that you can discuss with your GP, particularly if you cannot take oestrogen.
Talking Therapies
Speaking to a counsellor can be a helpful way to manage the anxiety, low mood, physical effects and lifestyle changes that can come with menopause.
During perimenopause, the levels of hormones in your body such as oestrogen, progesterone, and follicle-stimulating hormone (FSH) will change and they may fluctuate for a time. The overall fall of oestrogen means your menstrual cycle may get shorter or longer for a time before stopping.
It’s important to remember that as long as you’re still having periods, and indeed after your periods have stopped for up to a year, you can still get pregnant. If you want to prevent pregnancy you need to use contraception until you’ve had no periods for 12 months and have officially reached menopause.
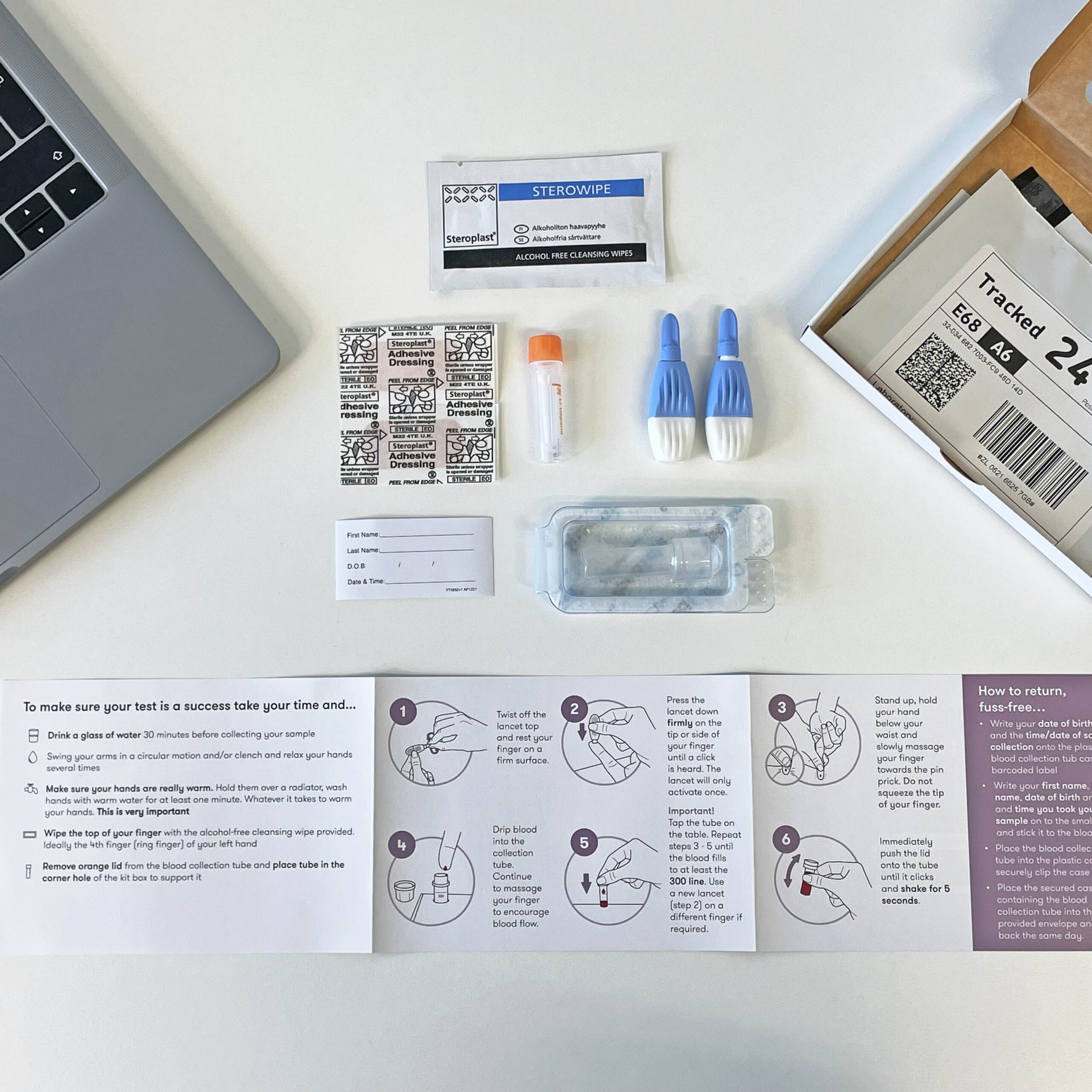
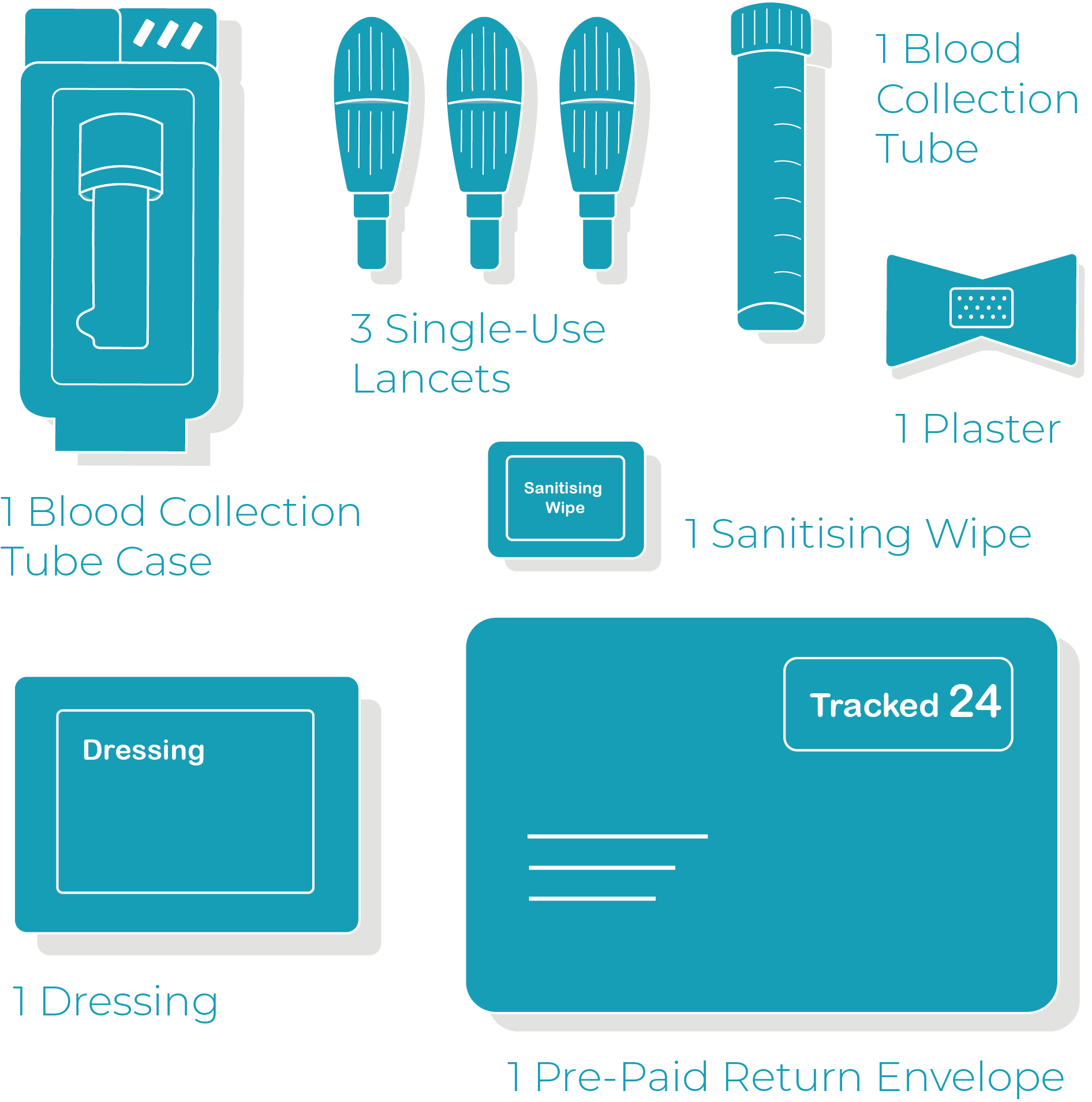
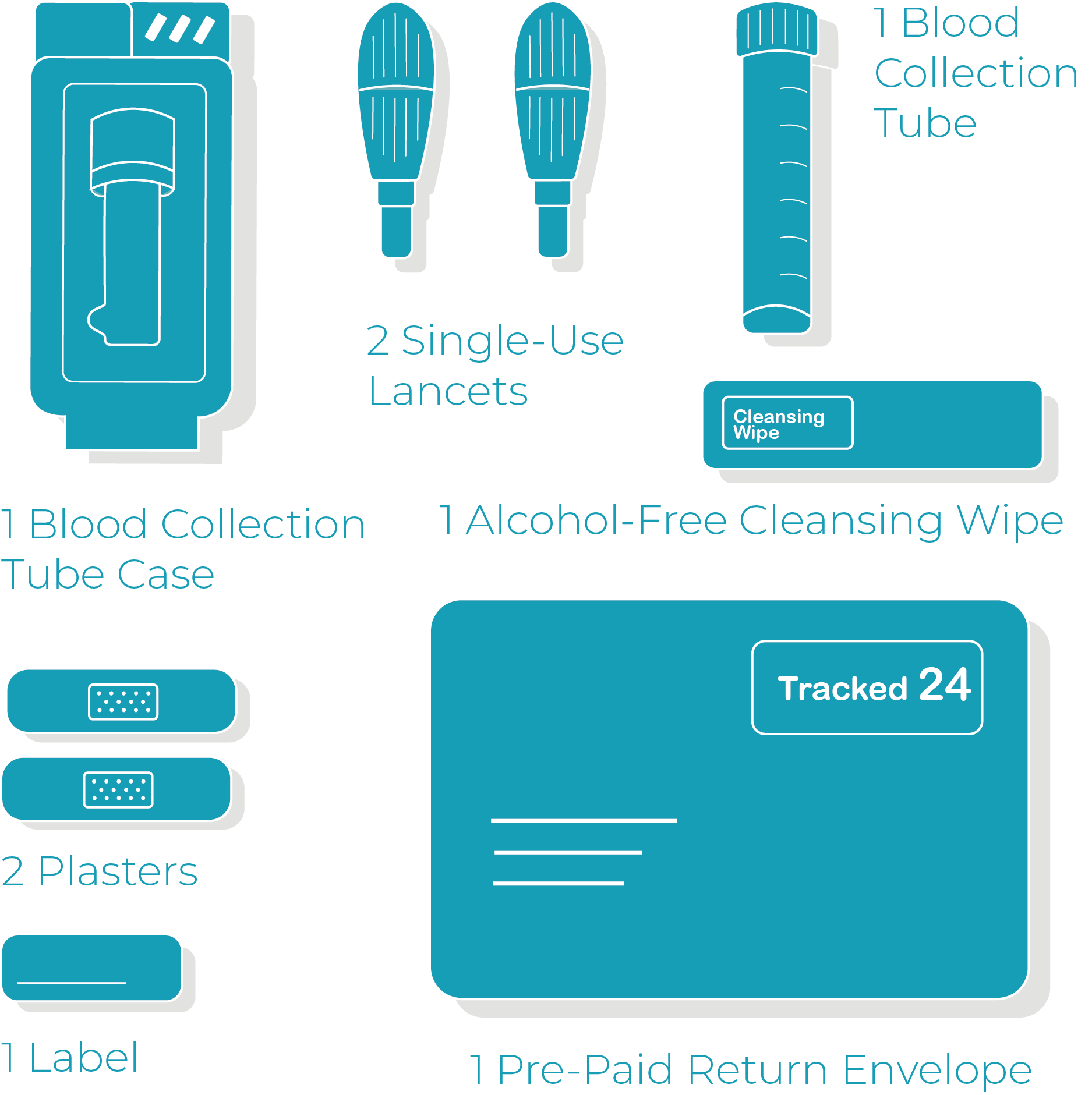
Whats In Your Test?
Our menopause test includes everything needed to take a blood test in the comfort of your own home, and return back to our laboratory for free. This ensures your sample is returned safely, and we’ll get straight to running a full analysis.
- A prepaid return envelope (England, Scotland, and Wales only)
- Two single-use lancets
- One blood collection tube
- One plastic blood collection tube case
- Two adhesive plasters
- A cleansing wipe
You May Also Like…
-
Sale!
Premium Food Intolerance Test
Original price was: £199.00.£139.00Current price is: £139.00. -
Sale!
Food Allergy Test
Original price was: £199.00.£139.00Current price is: £139.00. -
Sale!
Food Allergy & Intolerance Test Bundle
Original price was: £299.00.£249.00Current price is: £249.00. -
Sale!
Junior Food Intolerance Test
Original price was: £199.00.£139.00Current price is: £139.00.